|
“if the results of the imaging study could potentially change patient management, then the study is necessary. If interventions or outcomes are unlikely to be altered as a result of the imaging results, then the study is not needed.” (Magee et al) In sports, distal biceps tendon ruptures (DBTR) have been reported in to occur waterpolo, weightlifting, footballand gymnastics, and professional hockey player. The management of acute, complete distal biceps tendon ruptures is a surgical emergency, with improved prognosis and decreased risk of complications when surgery occurs within ten days of injury. Primary health care providers are often the first professionals to assess the acutely injured individuals and therefore, confidence in making a definitive clinical diagnosis of complete DBTR may prevent the inherent cost and time delay in obtaining “confirmatory” imaging. Clinical presentation and patient history are important factors in diagnosing complete DBTR. Rupture of the distal biceps tendon predominantly affects males within the 40 to 60-age range and typically occurs as a result of an eccentric contraction at the dominant elbow. Therefore, these injuries may occur in sports with a large extension force applied to the elbow from a concentrically flexed and supinated position (another reason why you shouldn’t do barbell curls), generally resulting in injury at the tendinous insertion to the radial tuberosity. Sometimes chronic in nature, injured patients often describe an acute traumatic event with hearing a “pop” or feeling sharp pain. Typically they are aware of the nature of their injury. Pain is often sharp and well localized, although dull and achy sensations have also been reported. Ecchymosis, swelling, and proximal retraction of the muscle belly are common signs in acute tendon ruptures though not always present. Orthopaedic tests for this DBTR have recently been described and individually have been accurate in detecting complete tendon ruptures. Elmaraghy et al described the Biceps Crease Interval and reported a sensitivity of 96% and diagnostic accuracy of 93% in 29 patients with a diagnostic threshold of an interval greater than 6.0cm or crease ratio greater than 1.2. A high interrater reliability of measuring the BCI was also reported (0.79). The Hook Test by O’Driscoll et al was reported to have 100% sensitivity and specificity (33 of 33 patients with complete DBTR) although interrater reliability data for this technique was not included. A positive Flexion Initiation Test has also been described in the literature although its requirement of attempting to flex a 10-pound weight in an acute symptomatic individual seems impractical and may not be clinically useful. Diagnostic imaging for distal biceps tendon ruptures are still commonly performed though may not entirely be necessary. With respect to diagnostic ultrasound, its utility seems questionable as diagnosis can be difficult in partial tears or complete ruptures without tendon retraction. In addition, sonography has been equivocal in cases of long-standing injuries with a delayed diagnosis. It may seem to play a role, however, in rare, atypical presentations; rupture without traumatic mechanism, clinically suspected partial tears, clinically suspected complete, non-retracted tears, and incomplete clinical pictures. Lastly, although relatively quick to obtain and of minimal cost, its accuracy is generally highly operator dependent. The detrimental risk of the time delay associated with obtaining an U/S may outweigh any potential benefit in addition to as appropriately applied clinical assessment protocol in most cases.
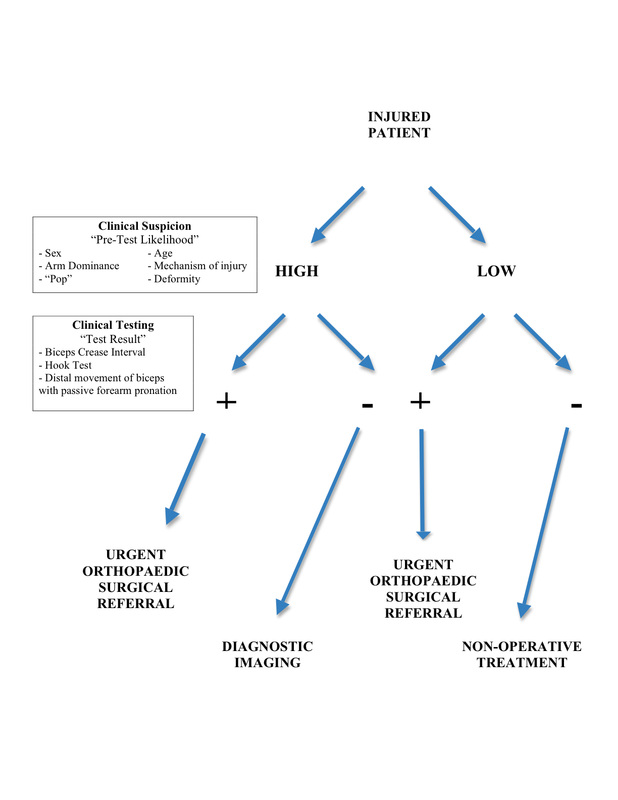
Magnetic resonance imaging is considered the gold standard imaging procedure in the detection of distal biceps tendon ruptures. It can also be useful in rare, atypical presentations such as clinically confusing cases where the biceps tendon can still be palpated in the antecubital fossa, as well as in complete non-retracted tears. In fact, the use of MRI in clinically confusing cases MAY lead to a change in the treatment protocol. Unfortunately however, MRI comes at an increased cost, decreased accessibility and lengthy wait times and this may negatively affect the prognosis of acute distal biceps tendon ruptures. Surgical delays greater than 10 days post injury increase the risk of complications and the extent of anterior dissection required. Therefore, in light of the questionability of ultrasound, and the expense and wait time of MRI, a a rapid and thorough clinical assessment protocol was developed, and and can be found below. This protocol MAY circumvent the need for diagnostic imaging, however, it must be noted that if either of sonography and MRI have the potential to change the treatment protocol as described in Magee above, then its use may be warranted.
0 Comments
Leave a Reply. |